Improve Billing Processes with an Optical Practice Management System
Different practices have different patient policies on when payments are due. But I’m sure that we can all agree that it is best when you can collect full payment as soon as possible. How well do you think your billing and collection process is working for your practice?
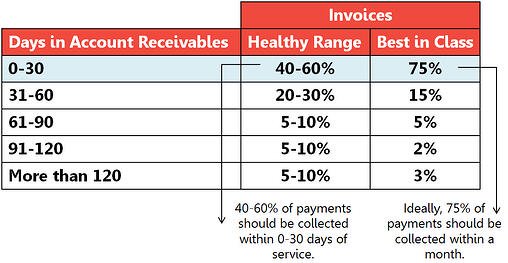
Find out how long your invoices sit in your accounts receivables uncollected, and how long it takes for you to be reimbursed by insurance payers. Then, use the table below to see how soon your payments should be collected. If you fall in the healthy range, you’re doing pretty well! But if you want to be best in class, use the following tips to see how an optical practice management system can further improve your billing and collection process!
Two Tips for Improving Your Billing Process
Using an Optical Practice Management System
Ensure Proper Coding
When a doctor makes a diagnosis and sends it to billing, the biller generating the claim should ensure that the ICD (primary diagnosis) supports the CPT code (procedure code). We’re sure that your biller is great at the job, but without a claims management system, claims can be prone to errors. And when a complicated optometry billing situation arises, it might be too time consuming for your biller to handle. Not only is a claims management system important, we think that it’s best if it’s embedded or integrated with your practice management system!
If you get a practice management system that has built in ICD codes, there should be error-checking features to make sure that your claims are accurate before submission. Proper coding prevents insurance denials and delayed payments. Your practice should also ensure that insurance billing is performed daily or, worst case, at a minimum, weekly.
Collect Full Payment as Soon as Possible
Collecting late payments from patients is no easy task. It’s always a difficult and awkward situation to face. To prevent that from happening, your front desk staff should use your practice management system to check for insurance eligibility and authorization before the patient proceeds to the exam room, and ideally before they book an appointment.
If there are issues with their insurance plan, you should explain what the charges would be without coverage before proceeding. If the patient’s plan comes with a co-pay, make sure that they are collected in full at the time of service.
We created a webinar to turn your denials into dollars. Improve your billing starting today.

