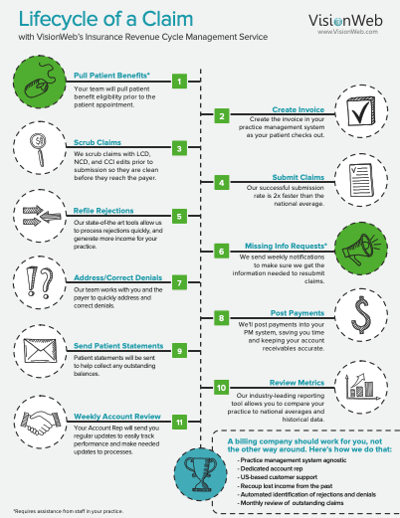
Infographic: Lifecycle of a Claim
"Efficiency" and "time-saving" are two of our top priorities when it comes to optometry software solutions and insurance claims processing services. We strive to make the OD's life easier by providing your team with top of the line services and streamlining your daily tasks.
One of the best ways to save time and money in your busy eyecare practice is to take advantage of VisionWeb's electronic claims processing services. Processing claims electronically has an endless list of benefits, including spending less time on the phone with payers, reducing redundancies of duplicate data entry, ensuring proper coding of claims, decreasing reimbursement times, and many more. While we are sure you are aware of all these benefits, have you ever wondered what the actual claim filing process looks like on our end?
The Claim Journey from Patient to Payment
If you want to know more about our processing claims or increasing your claim revenue, read our free insurance kit below.